If you have diabetes mellitus, your body does not use and store sugar properly. High blood-sugar levels can damage blood vessels in the retina, the nerve layer at the back of the eye that senses light and helps to send images to the brain. The damage to retinal vessels is referred to as diabetic retinopathy.
There are two types of diabetic retinopathy: nonproliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR).
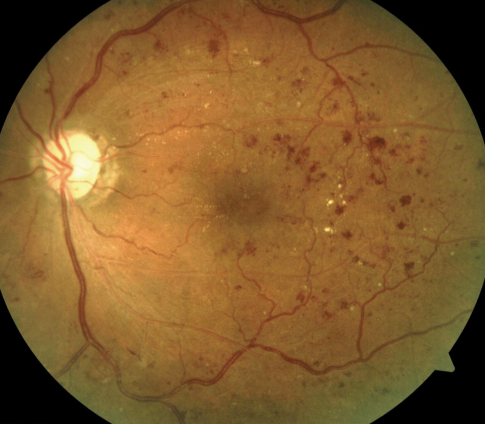
NPDR, commonly known as background retinopathy, is an early stage of diabetic retinopathy. In this stage, tiny blood vessels within the retina leak blood or fluid. The leaking fluid causes the retina to swell or to form deposits called exudates.
Many people with diabetes have mild NPDR, which usually does not affect their vision. When vision is affected it is the result of macular edema (pronounced eh- DEEM-uh) and/or macular ischemia (pronounced ih-SKEE-mee-uh).
Macular edema: This the is swelling or thickening of the macula, a small area in the center of the retina that allows us to see fine details clearly. The swelling is caused by fluid leaking from retinal blood vessels. It is the most common cause of visual loss in diabetes. Vision loss may be mild to severe, but even in the worst cases, peripheral vision continues to function.
Macular ischemia: This occurs when small blood vessels (capillaries) close. Vision blurs because the macula no longer receives sufficient blood supply to work properly.
PDR is present when abnormal new vessels (neovascularization) begin growing on the surface of the retina or optic nerve. The main cause of PDR is widespread closure of retinal blood vessels, preventing adequate blood flow. The retina responds by growing new blood vessels in an attempt to supply blood to the area where the original vessels closed.
Unfortunately, the new abnormal blood vessels do not resupply the retina with normal blood flow. The new vessels are often accompanied by scar tissue that may cause wrinkling or detachment of the retina.
PDR may cause more severe vision loss than NPDR because it can affect both central and peripheral vision.
Proliferative diabetic retinopathy causes visual loss in the following ways:
Vitreous hemorrhage: The fragile new vessels may bleed into the vitreous, a clear, gel-like substance that fills the center of the eye. If the vitreous hemorrhage is small, a person might see only a few new, dark floaters. A very large hemorrhage might block out all vision.
It may take days, months, or even years to reabsorb the blood, depending on the amount of blood present. If the eye does not clear the vitreous blood adequately within a reasonable time, vitrectomy surgery may be recommended.
Vitreous hemorrhage alone does not cause permanent vision loss. When the blood clears, vision may return to its former level unless the macula is damaged.
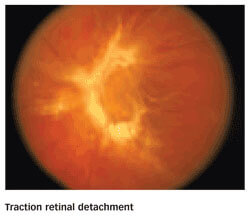
Traction retinal detachment: When PDR is present, scar tissue associated with neovascularization can shrink, wrinkling and pulling the retina from its normal position. Macular wrinkling can cause visual distortion. More severe vision loss can occur if the macula or large areas of the retina are detached.
Neovascular glaucoma: Occasionally, extensive retinal vessel closure will cause new, abnormal blood vessels to grow on the iris (colored part of the eye) and block the normal flow of fluid out of the eye. Pressure in the eye builds up, resulting in neovascular glaucoma, a severe eye disease that causes damage to the optic nerve.
A medical eye examination is the only way to detect changes inside your eye. An ophthalmologist (Eye MD) can often diagnose and treat serious retinopathy before you are aware of any vision problems. The ophthalmologist dilates your pupil and looks inside of the eye with an ophthalmoscope.
If your ophthalmologist finds diabetic retinopathy, he or she may order color photographs of the retina, a special test called fluorescein angiography, or a special scan called optical coherence tomography (OCT) to find out if you need treatment. Flourescein aniography is a test where dye is injected into your arm and photos of your eye are taken to detect where fluid is leaking. OCT is a high resolution scan of the retina to detect leaking fluid within or underneath the retina.
The best treatment is to prevent the development of retinopathy as much as possible. Strict control of your blood sugar will significantly reduce the long-term risk of vision loss from diabetic retinopathy. If high blood pressure and kidney problems are present, they need to be treated.
Laser surgery: Laser surgery is often recommended for people with macular edema, PDR, and neovascular glaucoma. Laser surgeries are performed in your doctor’s office.
For macular edema, the laser is focused on the damaged retina near the macula to decrease the fluid leakage. The main goal of treatment is to prevent further loss of vision. It is uncommon for people who have blurred vision from macular edema to recover normal vision, although some may experience partial improvement. A few people may see the laser spots near the center of their vision following treatment. The spots usually fade with time but may not disappear.
For PDR, the laser is focused on all parts of the retina except the macula. This panretinal photocoagulation treatment causes abnormal new vessels to shrink and often prevents them from growing in the future. It also decreases the chance that vitreous bleeding or retinal distortion will occur.
Multiple laser treatments over time are sometimes necessary. Laser surgery does not cure diabetic retinopathy and does not always prevent further loss of vision.
Injections of Medication Into the Eye: Injections of medications, live Avastin or steroids, into the eye are often used in combination with laser surgery to treat macular edema, PDR, and neovascular glaucoma. for macular edema, the injections can help decrease the leaking of fluid into the retina. For PDR and neovasular glaucoma, an injection of Avastin can often reduce the growth of abnormal blood vessels. These injections are all performed in your doctor’s office.
Vitrectomy: In advanced PDR, your ophthalmologist may recommend a vitrectomy. During this microsurgical procedure, which is performed in the operating room, the blood-filled vitreous is removed and replaced with a clear solution. Your ophthalmologist may wait for several months or up to a year to see if the blood clears on its own before performing a vitrectomy.
Vitrectomy often prevents further bleeding by removing the abnormal vessels that caused the bleeding. If the retina is detached, it can be repaired during the vitrectomy surgery. Surgery should usually be done early because macular distortion or traction retinal detachment will cause permanent visual loss. The longer the macula is distorted or out of place, the more serious the vision loss will be.
If you have diabetes, it is important to know that today, with improved methods of diagnosis and treatment, only a small percentage of people who develop retinopathy have serious vision problems. Early detection of diabetic retinopathy is the best protection against loss of vision.
You can significantly lower your risk of vision loss by maintaining strict control of your blood sugar and visiting your ophthalmologist regularly.
People with diabetes should schedule examinations at least once a year. More frequent medical eye examinations may be necessary after a diagnosis of diabetic retinopathy.
Pregnant women with diabetes should schedule an appointment in the first trimester, because retinopathy can progress quickly during pregnancy.
If you need to be examined for eyeglasses, it is important that your blood sugar be consistently under control for several days when you see your ophthalmologist. Eyeglasses that work well when blood sugar is out of control will not work well when blood sugar is stable.
Rapid changes in blood sugar can cause fluctuating vision in both eyes even if retinopathy is not present.
You should have your eyes checked promptly if you have visual changes that:
When you are first diagnosed with diabetes, you should have your eyes checked:
You’ll see that when it’s time to make an appointment with a specialist in Retina and Vitreous diseases, you can trust your eye health to the team at Inland Valley Retina Medical Associates, Inc.